Uncover the early stages of autoimmune type 1 diabetes
The science of understanding the presymptomatic stages of type 1 diabetes (T1D) has expanded – your doctor may be able to help detect early stages of autoimmune T1D long before any signs or symptoms begin.
The information provided is for educational purposes only and does not construe medical advice. Screening decisions should always be made in consultation with your doctor.
Where would you like to start?




FAQ=frequently asked questions.
Autoimmune type 1 diabetes is a chronic, progressive autoimmune disease
What does this mean?
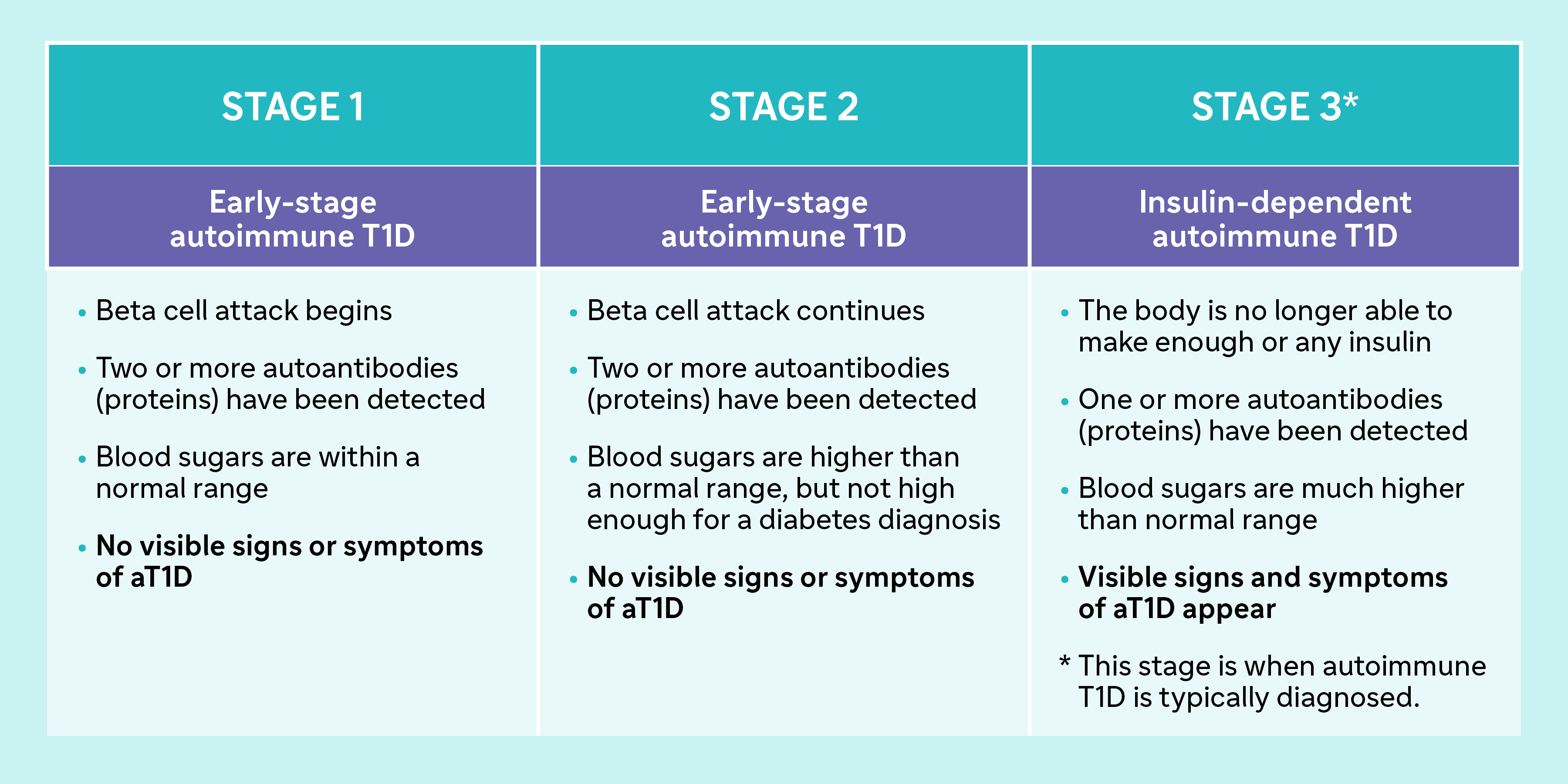
Autoimmune T1D is a life-long condition that progresses in three distinct stages.
The immune system’s role is to protect the body from harmful threats. An autoimmune disease occurs when the immune system mistakenly targets and attacks healthy cells. In autoimmune T1D, the immune system attacks healthy cells in the pancreas called beta cells. This immune attack can be initiated by an infection or other triggers. The tendency to develop an autoimmune condition can also be inherited from your parents.
 |
The role of beta cells and insulinBeta cells are responsible for producing insulin, an important hormone that transports blood sugar (glucose) where it’s used for energy. Why is insulin so important?Without enough insulin, sugar cannot be properly used by the body, resulting in high blood sugar levels. Autoimmune T1D can be asymptomatic or have subtle signs that go unnoticed for a period of time before the symptoms become more apparent. |
What is DKA?
When someone is unaware of being in the early stages of autoimmune T1D, they may be at risk in the future of a DKA event.
When insulin is low, the body is unable to get enough blood sugar into its cells. The body will break down too much fat, which is not good for our bodies and makes the blood acidic, known as ketoacidosis.
As the acidity level goes up, there is a risk of developing severe complications like fluid building up in the brain, the heart stopping and kidney failure.
Sanofi is not providing medical advice. If you have more questions, please discuss the risk of complications of DKA and its symptoms with your healthcare provider.
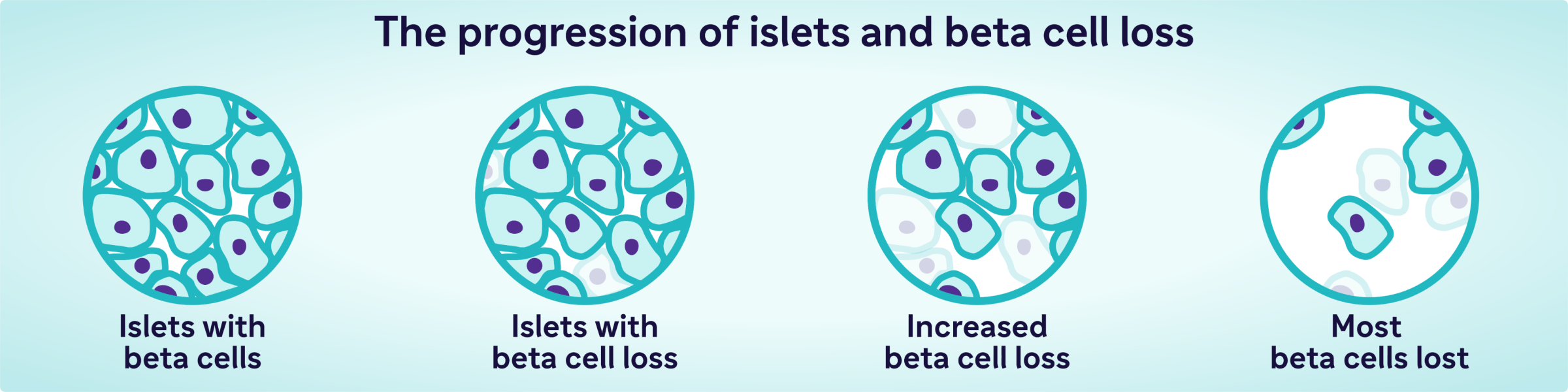
Understanding the progression of autoimmune T1D
Early-stage autoimmune T1D occurs when the immune system has started attacking the beta cells, but the body is still able to produce enough insulin to maintain blood sugar levels within a relatively healthy range.
The attack on beta cells can be detected by the presence of a group of proteins called islet autoantibodies. Some of these autoantibodies can be detected by tests ordered through your doctor. Participants in research programs like TrialNet have access to 4 autoantibody tests from sources like the US.
Autoimmune T1D progresses in 3 stages
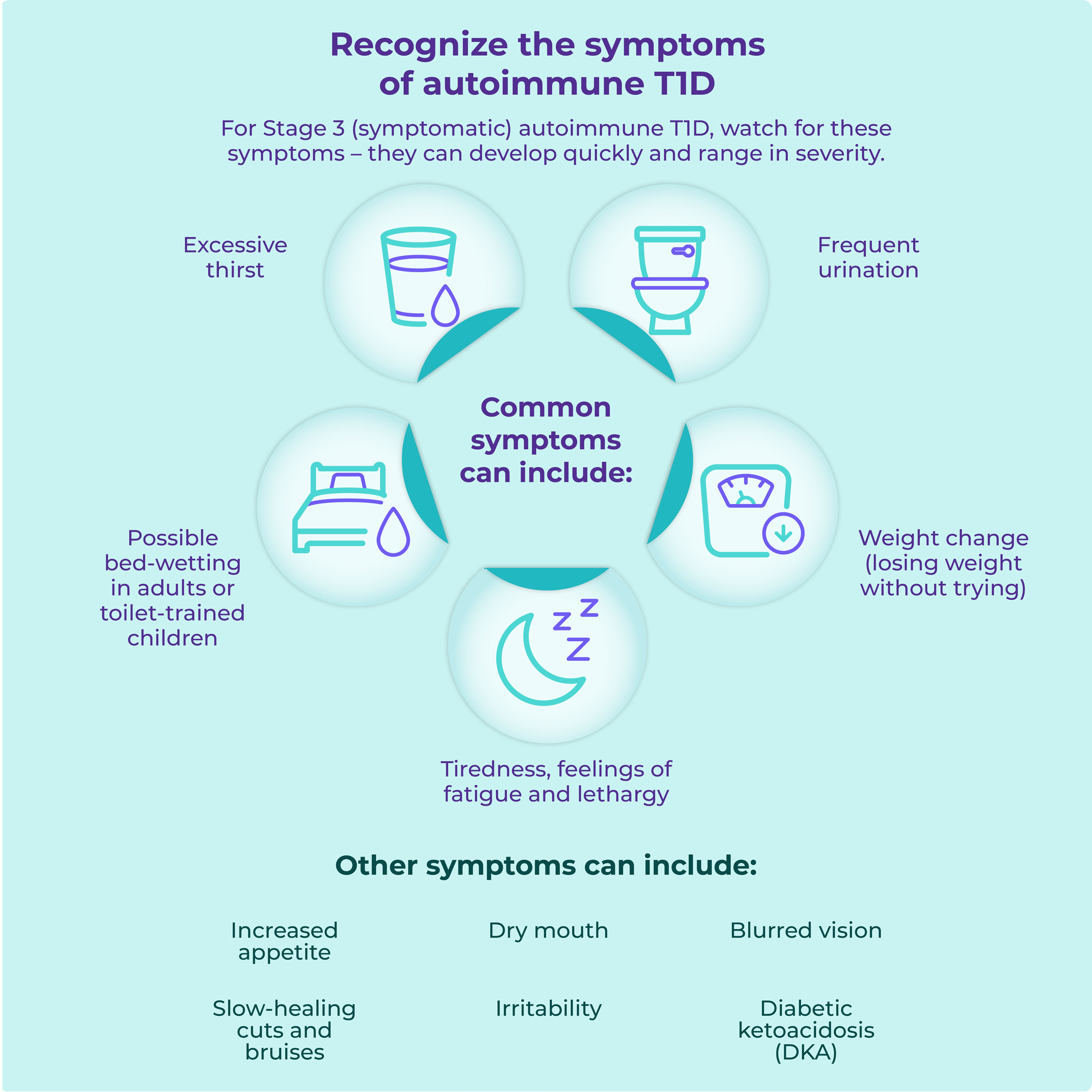
Recognize the symptoms of autoimmune T1D
For Stage 3 (symptomatic) autoimmune T1D, watch for these symptoms – they can develop quickly and range in severity.
Common symptoms can include:
- Excessive thirst
- Frequent urination
- Possible bed-wetting in adults or toilet-trained children
- Weight change (losing weight without trying)
- Tiredness, feelings of fatigue and lethargy
Other symptoms can include:
- Increased appetite
- Dry mouth
- Blurred vision
- Slow-healing cuts and bruises
- Irritability
- Diabetic ketoacidosis (DKA)
Symptoms such as excessive thirst, frequent urination, and lack of weight gain or weight loss can be difficult to recognize.
These subtle symptoms may be mistaken for a growth spurt or changes in thirst due to changes in routine (such as school) or weather changes. Parents may also not notice that their child is urinating more frequently at school or during the night. If you notice these changes, be sure to discuss these issues with your or your child’s healthcare professional.
If you have questions about T1D development or the risk of DKA for yourself or a family member, speak to a healthcare provider
Detect autoimmune T1D today
A blood test can determine an individual’s overall risk for developing autoimmune T1D
Autoantibody blood tests can proactively detect autoimmune T1D in Stage 1 or 2 – before you have symptoms.
Detecting two or more of these autoantibodies suggests the early stages of autoimmune T1D. The test is typically done with a finger prick or blood draw.
Proactively screening for autoantibodies associated with Stage 1 and Stage 2 autoimmune T1D can help determine your overall risk for progressing to Stage 3 autoimmune T1D.
Screening for autoimmune T1D is also important in helping to reduce the occurrence of DKA. Healthcare professionals may be able to monitor those individuals sooner and manage their symptoms to help prevent DKA.
Diabetes Canada and Breakthrough T1D both recognize the importance of identifying early-stage autoimmune T1D.
By knowing if you or a member of your family is in the early stages of autoimmune T1D, you can be better prepared to recognize symptoms when they appear.
Consult your or your family member’s healthcare provider to discuss how you may be able to detect autoimmune T1D early. This can help you understand what's ahead and lower the risk of potentially life-threatening complications, like DKA, with a doctor's help.
How can you get screened in Canada?
Request a screening kit from the TrialNet Research Program
You can sign up for a screening kit if you have a first-, second- or third-degree relative with autoimmune T1D through the TrialNet Research Program.
This program offers autoimmune T1D risk screening through a simple blood test that detects T1D-associated autoantibodies.
Ask a healthcare provider
Your family healthcare provider may be able to offer screening through their clinic or a lab. Talk to them for more information.
CanScreenT1D
Breakthrough T1D, in collaboration with Canadian Institutes of Health Research, has announced the launch of CanScreenT1D – a Canadian research initiative that is exploring the possibility of general population screening for early-stage autoimmune T1D. The pilot screening program is estimated to start in 2026.
Currently, general population screening is not recommended in Canada.
Talk to your family healthcare provider about early detection